In early September 2019, I was dropped from care by my medication assisted treatment (MAT) program — a highly effective treatment for opioid addiction that uses medication to rebalance brain chemistry and mitigate withdrawal and cravings — because I had the flu.
I was biking to treatment three to five days a week in the Florida heat, and had no other transportation, so I wasn’t able to come in for dosing after I came down with a fever and a deep, phlegmatic cough. But I called in, emailed, and texted each day that I missed a scheduled day of treatment. At no point was I warned of an impending discharge; my counselor simply wished me well, and suggested I go to urgent care if I felt I needed it.
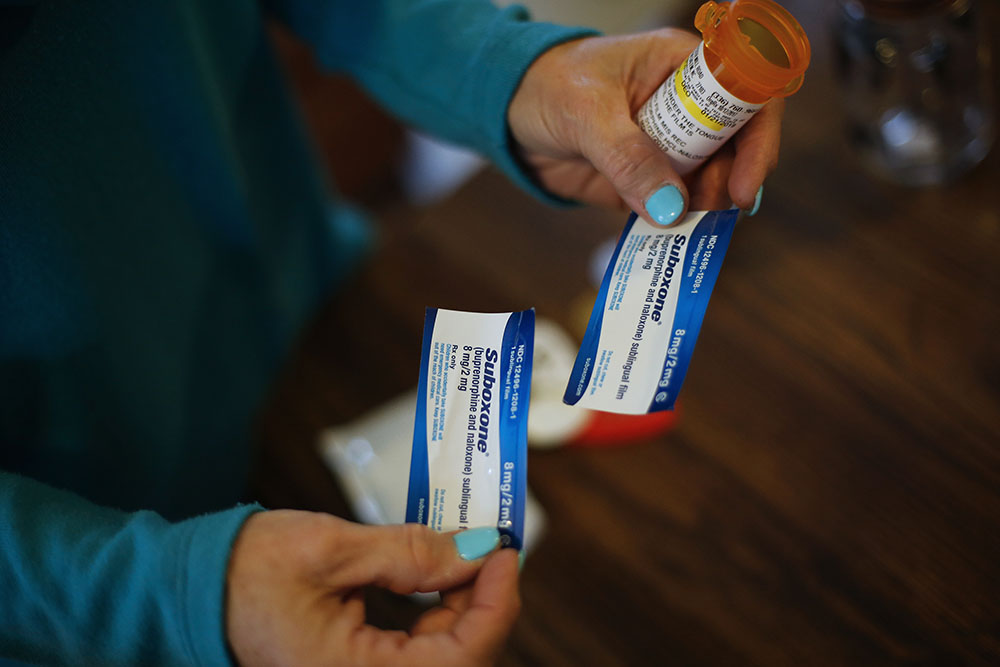
When I returned to treatment the next week, though, I learned that my provider, Memorial Outpatient Behavioral Health, had assumed I was skipping to use drugs. They dumped me without even a few days’ supply of my prescribed buprenorphine, upon which my body was physically dependent; a referral elsewhere; or a solid reason.
This was in spite of my having an active prescription from my doctor and a future appointment with her. I could also no longer access the psychiatric medication I was prescribed through the same provider.
Get Talk Poverty In Your Inbox
All of a sudden, without warning, I lost all of my addiction and mental health care. As shocking as these events have been, they are not uncommon. In fact, they represent a dangerous status quo among opioid addiction treatment providers across the nation, one that defies all modern research on addiction treatment and leaves patients stranded.
“It’s an old school type of thinking which came out of how we’ve treated addiction in the past, which is that abstinence is the policy, which doesn’t make sense with a chronic relapsing disease,” said Justine Waldman, the medical director for REACH, a harm-reduction oriented health hub in Ithaca, New York. “With abstinence being the policy, once the patient isn’t able to follow the policy the patient isn’t able to be part of the practice.”
Keri Ballweber, a methadone patient and recovery specialist at Point to Point Kane County, remembers being dramatically dropped from care in 2012 by Family Guidance Center, a methadone provider in Aurora, Illinois with whom she had been a patient for roughly six and a half years. In the two years prior to her discharge, she had been gradually tapering her 160 mg dose with the goal of coming fully off methadone.
“As I got lower in my taper, it began getting harder and harder to deal with the symptoms [of withdrawal],” recalled Ballweber. “I asked them for help, but their only suggestion was to go slower. It did not seem as if there was a speed slow enough to not cause me discomfort.” Family Guidance Center declined to comment for this piece; Memorial Outpatient Behavioral Health said it does not comment on specific cases, but that “our goal is to partner with all our patients and help them heal and recover.”
Ballweber eventually turned to illegally purchased diazepam, a benzodiazepine usually prescribed for anxiety, insomnia, and seizure disorders. Mixing benzos and opioids can be dangerous, but when Ballweber disclosed the use to her counselor, she was not informed about this, nor given any harm reduction tips. She asked if she could be kicked out of the program if she continued to screen positive for the non-prescribed drug, and her counselor admitted that outcome was possible, but assured her that such a drastic action would only be taken much further down the line.
The next month, Ballweber was dismissed, and tapered from her dose within a week.
“I was very sick,” said Ballweber. “I couldn’t sleep, I was having panic attacks, muscle tremors, [and] restless leg syndrome.” Eventually, she began to experience hallucinations, which she believes were the result of sleep deprivation from the withdrawal. She was admitted to the hospital for psychosis and prescribed quetapine, an anti-psychotic medication, which helped her sleep. “I had absolutely no aftercare and cutting me off from the clinic [also] cut me off from counseling,” she said.
Ballweber also recalls seeing other patients discharged or punished with medication holds for talking back to their counselors or smoking too close to the buildings. Other MAT patients around the country have reported being dropped or threatened with dismissal for reasons such as relapsing, missing care for unavoidable reasons like being incarcerated, not attending group therapy sessions, smoking marijuana, or being unable to pay.
In my case, when the clinic refused to give me my prescribed medication, leaving me in opioid withdrawal and overcome by a sense of deep confusion and hopelessness, I did eventually use. It was a bad choice, I admit that — and I told my counselor immediately. But in many ways, the clinic itself had contributed to the outcome it had initially accused me of.
– Mary Jeanne Kreek
I think a part of me hoped that if I gave them what they expected — a positive toxicology screen — I would get what I needed: ongoing care. Instead, I was totally shut out and sent to navigate detoxing from both my opioid-based buprenorphine and my selective serotonin reuptake inhibitor antidepressant (also dependency-producing) at home, alone, with no medical supervision or follow-up care.
Both buprenorphine and methadone are approved by a slew of licensing bodies, including the World Health Organization, as the most effective treatments for reducing harmful symptoms of opioid addiction and opioid addiction-related deaths. Although any addiction treatment plan should be tailored to the individual patient’s needs and circumstances, these medications are designed for long-term or even lifelong use, said Mary Jeanne Kreek, senior attending physician at Rockefeller University’s addictive diseases lab and part of the team that first developed methadone as a treatment for addiction, whom I interviewed while researching a story for Filter Mag. No part of best practice includes suddenly dropping patients from care for any reason — but especially not for showing symptoms of the disorder for which they are seeking care.
“I’m afraid for any patient who has to get off MAT before they’re ready,” added Kreek.
For patients who relapse, Waldman confirmed the best practice is to “keep the patient on buprenorphine.”
At REACH, she noted, patients are not expected to adhere to an abstinence-only model of care. When patients continue to relapse, their practitioners sit down and ask the patients what they need and how they can help.
“There have only been two patients that I can think of who weren’t able to get care at REACH,” she said, “and they were displaying more violent behavior that just didn’t feel safe within our workplace.” She makes a point to add that REACH ensured those patients were placed with a more appropriate provider.
Losing access to medication also affected my ongoing child services case, switching it from a reunification track to one in which my children will be given up for adoption due to an assumption by my caseworkers and my judge that I am at fault for “failing” treatment. This doesn’t guarantee that I will permanently lose my two young daughters, but it makes it a much tougher battle to win. Now, I am no longer entitled to the little assistance I was receiving from my local child welfare agency in obtaining the services I need to reunify with my daughters. They are oriented toward settling my daughters into permanency with their grandparents.
When I told my counselor that this would happen if they dropped me from care, she responded that she thought I should get my daughters back, and was probably a great mother, but was not a dedicated enough patient.